Article by Hannah Roberts, National Assembly for Wales Research Service
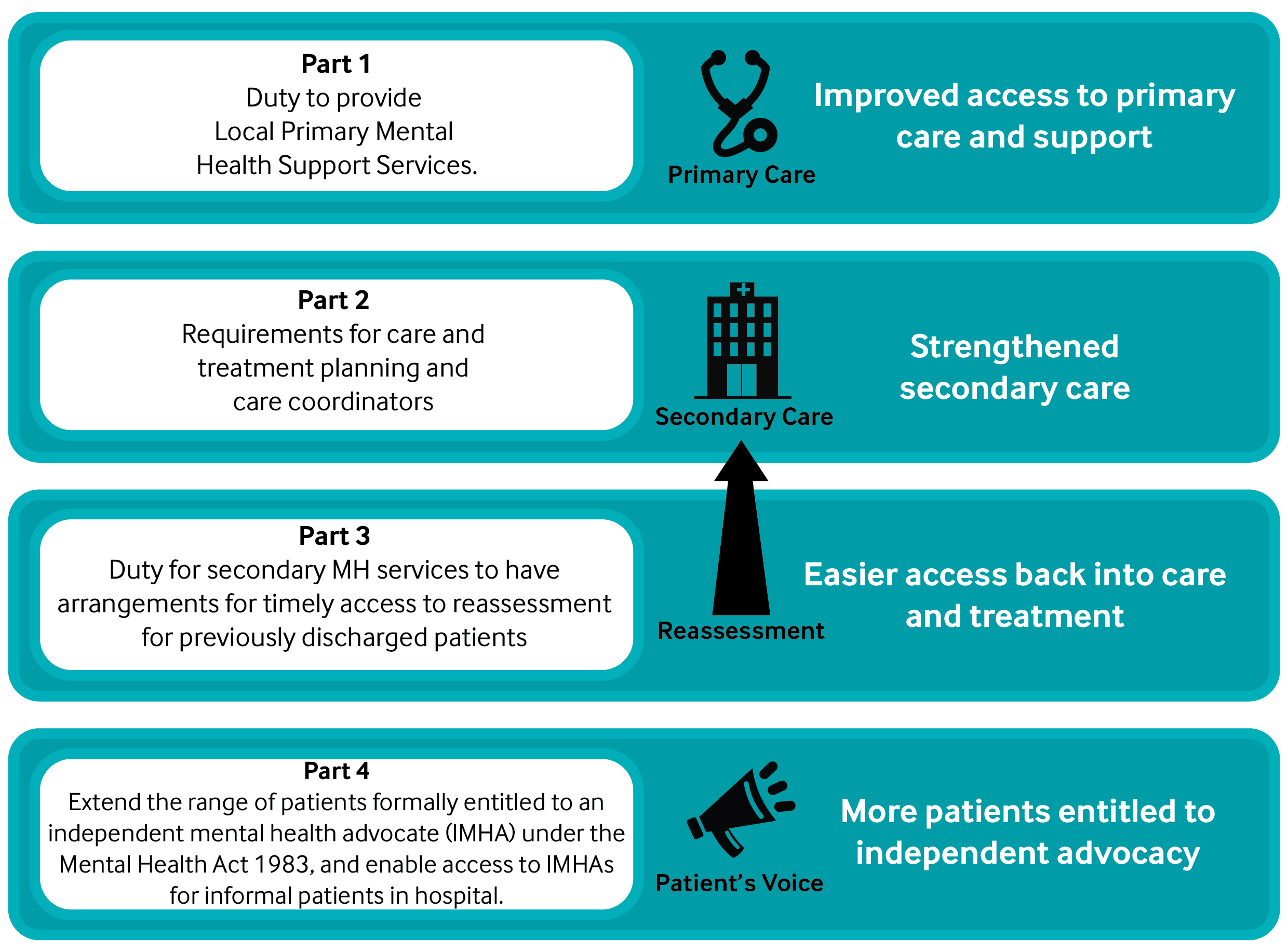 The Mental Health (Wales) Measure 2010 was implemented in phases between Jan-Oct 2012. Its aims were to secure earlier and easier access to services for people with mental health (MH) problems. The Measure is summarised in the diagram below. More details can be found in this public summary leaflet on the Measure. The Welsh Ministers had a duty to review the Measure within 4 years of commencing implementation. The inception report described in detail how this evaluation would be carried out. An interim report was issued in 2014 and stated that
The Mental Health (Wales) Measure 2010 was implemented in phases between Jan-Oct 2012. Its aims were to secure earlier and easier access to services for people with mental health (MH) problems. The Measure is summarised in the diagram below. More details can be found in this public summary leaflet on the Measure. The Welsh Ministers had a duty to review the Measure within 4 years of commencing implementation. The inception report described in detail how this evaluation would be carried out. An interim report was issued in 2014 and stated that
[…] the pace of change required has presented services in some areas with challenges. Whilst the same legislation and guidance applies across Wales, local need and the previous configuration of services have influenced the implementation of the Measure.
Review report
The duty to review final report, published in December 2015, states that all health boards and local authorities are complying with the legal requirements of the Measure. The remaining findings of the report, on to what extent the implementation of the Measure is achieving its aims, are summarised below. The report concluded that the change in culture required to ensure the intention behind the Measure is becoming more evident across Wales. It states that while there is room for ongoing improvement, health boards have given increased priority and focus to mental health.
Part 1: Local Primary Mental Health Support Services (LPMHSSs)
LPMHSSs, located within and alongside GP services, are meeting a significant, previously unmet demand. There is concern that this high demand is placing a strain on services and resulting in longer waiting times, particularly for psychological (or ‘talking’) therapies Waiting times for assessment have decreased over the past two years and are now on target, whereas waiting times for an intervention are variable. Currently only 71% of patients commence their treatment within 28 days (target of 80%). This issue was raised by the Health and Social Care Committee’s post-legislative scrutiny of the Measure in 2014, and a national plan for the delivery of psychological interventions was developed in 2015. The review report recommends that data on waiting times for psychological interventions are routinely captured to monitor progress. It also notes a need to address the eligibility criteria for those able to undertake LPMHSS assessments. There will be a consultation on draft changes to the criteria in 2016. The report found that a positive knock-on effect of Part 1 of the Measure has been a ‘significant expansion in the availability of self-referral psychological education programmes’, also known as Tier 0 services.
Part 2: Care and treatment plans
The target was that 90% of individuals receiving secondary MH services should have a Care and Treatment Plan (CTP), and this is being met by all but one health board. The report notes that the quality of CTPs varies, and not all service users feel involved in the development of their CTPs. There are reported concerns that the bureaucracy involved in producing CTPs is creating barriers between primary and secondary care and impacting on the time that practitioners have for patient care. The report recommends that the form and content of CTPs be reviewed, and there have been calls for further training of care coordinators. The eligibility criteria for who can take on the role of care coordinator are being reconsidered and further guidance regarding what constitutes competency for the role has been recommended. There have been suggestions that the involvement of carers may also improve the quality of some CTPs, and there is work to be done in increasing the numbers of patients that are offered their CTP in Welsh or a language of their choice.
Part 3: Self-referral to secondary services
The report states since the implementation of Part 3, self-referral to secondary MH services by patients who were previously discharged has become easier, though it is unclear whether the increase in self-referrals has led to a corresponding reduction in emergency admissions and assessment. There are doubts as to whether timely reassessment of patients is being achieved; the report notes that more performance indicators need to be collected to measure this. It also states there is still a lack of information and understanding, amongst patients, GPs and secondary care practitioners, about the right to self-referral.
Part 4: Independent Mental Health Advocacy services
168 people per month now receive an independent mental advocacy service that was not available prior to the Measure. While the Measure has resulted in increased clarity and improved access to advocacy services, the reported uptake in general hospital settings is low. This is thought to be due to inadequate levels of awareness among healthcare staff; in one survey, 42% of patients felt that ward staff did not give an explanation of their entitlement to advocacy. The report notes that work also needs to be done on enabling access for those who lack the capacity to request it.
Children and young people
[caption id="attachment_5753" align="alignright" width="300"] Image from flickr.com by Joe Houghton. Licensed under the Creative Commons[/caption] The Health and Social Care Committee reported in their post-legislative scrutiny that the issue of ‘greatest concern’ was that children and young people were not benefitting fully from the Measure. On this issue, the review report states that provision under Part 1 will be addressed within the Together for Children and Young People initiative, which was launched in February to review Child and Adolescent Mental Health Services (CAMHS). An update on the CAMHS review is included in a written statement on mental health services in Wales, 7 October 2015. The report also recommends that Part 3 be amended to include children and young people in order to comply with the UN Convention on the Rights of the Child. The Assembly Children, Young People and Education (CYPE) Committee carried out an inquiry into Child and Adolescent Mental Health Services (CAMHS) in 2014. Further information can be found on the Committee’s webpage.
Image from flickr.com by Joe Houghton. Licensed under the Creative Commons[/caption] The Health and Social Care Committee reported in their post-legislative scrutiny that the issue of ‘greatest concern’ was that children and young people were not benefitting fully from the Measure. On this issue, the review report states that provision under Part 1 will be addressed within the Together for Children and Young People initiative, which was launched in February to review Child and Adolescent Mental Health Services (CAMHS). An update on the CAMHS review is included in a written statement on mental health services in Wales, 7 October 2015. The report also recommends that Part 3 be amended to include children and young people in order to comply with the UN Convention on the Rights of the Child. The Assembly Children, Young People and Education (CYPE) Committee carried out an inquiry into Child and Adolescent Mental Health Services (CAMHS) in 2014. Further information can be found on the Committee’s webpage.
The experiences and opinions of patients and healthcare professionals
Patient satisfaction
90% of those receiving LPMHSS rated the services positively and most patients surveyed found their GP extremely or very understanding. On the other hand some patients have reported limited support or interventions that did not meet their needs. Independent research found a range of experiences of reassessment – some patients felt it had been straightforward whereas others had encountered barriers to timely assessment.
Healthcare professionals’ perspective
The report notes that collating the opinions of healthcare professionals has been more difficult, with low response rates to surveys. 74% of GPs rated the LPMHSS positively, but as a result of the Measure GPs and primary care staff feel they have an increased work load, and many find this work difficult. Most GP practice staff surveyed said ‘they had hoped to learn more about how to manage patients with mental illness’. The report recommends that support and advice for GPs and other primary care staff is prioritised.






